This article is the first of a 3-part series where we explore all things physician efficiency, starting with the “why”.
At ReMedi Health Solutions, our Physician Informaticists have coached and trained practicing physicians in EHR efficiency and Personalization for over 15 years. We’ve seen it all—happy doctors, frustrated informatics teams, and passionate, curious super users. Over the past years, Team ReMedi, led by Dr. Sonny Hyare and Dr. Rajeeb Khatua, has developed a novel hybrid model to improve physician performance. We call our approach: Physician Efficiency Sessions. In short: these are highly tailored and custom EHR Personalization sessions conducted by physicians.
Each session builds upon early-stage Personalization methods that are typically conducted before and during the implementation of a new EHR system (e.g. Epic, Oracle Health). However, ReMedi’s model expands into focused, peer-to-peer efficiency coaching sessions that are specialty-specific. This approach not only enhances EHR proficiency but also addresses the broader issue of physician inefficiency in healthcare.
The Hidden Costs of Physician Inefficiency
Impact on Patient Care
When it comes to physicians underperforming due to the EHR, most would begin crunching the numbers surrounding the impacts to the health system’s bottom line. While the numbers are not small (we will review them later) let’s not forget the real priority in the equation: the patients.
Patient satisfaction plunges when simple expectations cannot be achieved. At ReMedi, we stress the importance of not allowing the EHR to hinder patient care. When health systems as a whole responsibly deliver care that prioritizes elements such as dignity, autonomy, prompt service and achievement of patient expectations – patients from all walks of life win. Health systems achieve less wait times, greater patient satisfaction scores, and happier clinicians when the EHR is leveraged efficiently.
Physician Burnout
The link between inefficient EHR use and physician burnout is well-documented. According to recent reports from KLAS Research and the Arch Collaborative, 34% of physicians report some level of burnout, with 54% of these burned-out physicians citing the EHR as a major contributor. Burnout not only affects physicians’ well-being but also their ability to provide optimal care.
As healthcare IT leaders, it’s important that we identify solutions that directly combat some of the leading causes of physician burnout:
- Staffing shortages
- Afterhours workload
- EHR inhibits efficiency and quality
- No control over workload
Doctors that receive EHR Personalization support from a peer report higher efficiency and less burnout. The need for using personalized EHR tools is critical: the doctors using optimized Note Templates, Order lists and Sets, Macros, Filters, Report views experience faster documentation and less burnout.
Regarding implementation and Go-Live, it’s important for physicians to start using the new system efficiently. Generally, classroom training isn’t designed to maximize efficiency. When a physician starts off using the EHR with a peer that coaches them based on their desired workflows, it increases user satisfaction and increases system adoption.
Financial Implications
Physician burnout has significant financial repercussions for healthcare organizations. Based on a study from the National Bureau of Economic Research, the cost of turnover caused by burnout and inefficiency is estimated at $87,000 per physician. KLAS and the Arch Collaborative’s survey efforts identified 4,279 physicians reporting EHR-related burnout, translating to around $372 million in financial risk.
Personalized EHR Training: Quantifiable Improvements in Healthcare Delivery
Evidence Supporting Personalization Techniques
Basic training and classroom style sessions are useful for the basics of EHR functionality. However they won’t improve chart-closure rates, nor decrease after-hours charting and burnout. In fact, 98% of UTHealth physicians that received Personalization with ReMedi felt more confident using Epic before Go-Live.
As former clinicians, the team at ReMedi recognizes the fact that physicians can be, well, nuanced. For this reason, we find that 1-on-1, peer-to-peer training is the most effective format to improve the efficiency of physicians. As referenced in the levels of training below, peer-to-peer training is the deepest level of training possible and creates the highest likelihood of increased EHR satisfaction for physicians.
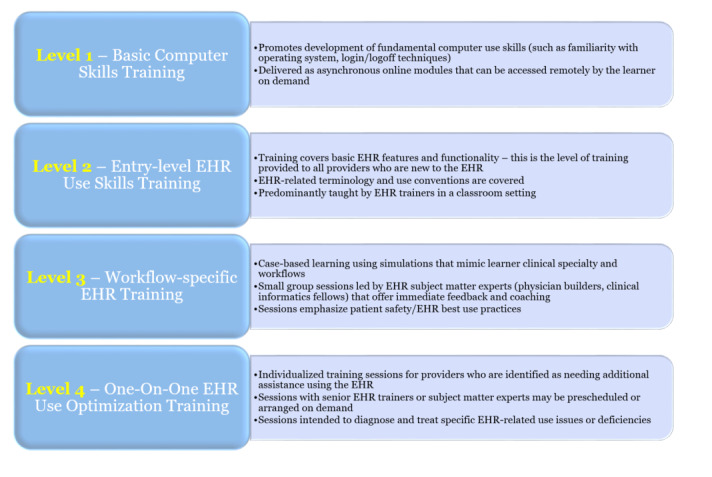
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8491113/
We find that peer-to-peer physician training does more than just build essential skills. It fosters a culture of collaboration across the entire health system. This approach creates best practices and yields improvements in documentation quality, efficiency, and overall clarity of the system. By focusing on physician empowerment and system optimization, our Personalization sessions give providers back what they lack most: time.
By tailoring the EHR training session to the specific needs and workflows of each physician, they become more proficient and comfortable with the system, leading to increased satisfaction and productivity.
Functions of the ReMedi Physician Efficiency Program and Personalization Sessions
- Continuing EHR Education: Ongoing training ensures physicians stay updated with the latest features and best practices.
- Improving Clinician Wellness: Efficient EHR use reduces stress and workload, contributing to better mental health.
- Peer-to-Peer Training: Physicians training physicians fosters a more relatable and effective learning environment.
- Workflow-Specific Training: Tailored training addresses the unique challenges of different specialties.
Implementing a Culture of Clinician Wellness
Creating a culture that prioritizes clinician wellness is essential for maintaining a happy and productive workforce. Addressing EHR inefficiencies is a critical component of this culture shift. By investing in personalized EHR training, healthcare organizations send a signal to its workforce that they are committed to providing adequate resources and supporting a path to success.
Why Health Systems Must Invest in EHR Personalization
Long-Term Benefits
Investing in personalized EHR training offers a substantial return on investment. Improved efficiency leads to cost savings, better patient outcomes, and increased physician retention.
The goal of creating more efficient doctors is not just financial ROI. For physicians, an increase in EHR efficiency dramatically improves job satisfaction, yields less burnout, and increases happiness in and out of the clinic. Overtime, the improvement in physician performance becomes the rising tide that lifts all the other boats (patients, healthcare systems, vendors, start-ups, etc.).
Competitive Advantage
Healthcare organizations that prioritize physician efficiency and wellness position themselves as leaders in the industry, attracting top talent and enhancing their reputation. Moreover, it improves the health system’s reputation among its patients. When a health system’s EHR processes are streamlined, it leads to more accurate documentation, directly impacting quality scores and reimbursement rates. The end-result of EHR efficiency is cultivating a continuous cycle of improved care quality and financial performance.
Regulatory Compliance
Health systems that prioritize EHR efficiency achieve greater levels of regulatory compliance, including more accurate reporting and reducing the potential for issues. We find that when focus is placed on accurate documentation practices, errors go down. By optimizing EHR workflows, organizations can more easily meet requirements for quality reporting. This efficiency also leads to more accurate clinical documentation and precise coding, reducing compliance risks while improving reimbursement through better case mix index and fewer claim denials. In the long-run, streamlined EHR workflows enable robust data analytics, supporting population health management and easier adaptation to evolving regulatory frameworks like MIPS, HCCs, APMs, and others.
Conclusion
Physician inefficiency, particularly with systems like Epic and Oracle Health, has far-reaching implications—from decreased patient satisfaction to significant financial losses due to burnout. ReMedi Health Solutions’ Physician Efficiency Sessions and Personalization solution offer a proven solution to these challenges. By investing in personalized, peer-to-peer EHR training, healthcare organizations can enhance physician efficiency, improve clinician wellness, and ultimately provide better patient care.
Schedule a ReMedi Personalization Program Demo
We invite health system leaders to schedule an interactive demo to better understand how ReMedi’s Personalization program can be implemented to improve physician performance and satisfaction. Visit this link to schedule a demo.
In our next article, we’ll delve into how our unique approach to physician efficiency works and why it stands out in the industry.