A Strategic Guide for Health Systems and Epic Consulting Teams
Epic Systems is the leading electronic health record platform for large health systems, academic medical centers, and integrated delivery networks. Its strength lies in a unified suite of modules that share a single patient record across clinical, operational, and financial workflows. For healthcare leaders, understanding the structure of Epic’s ecosystem is essential to guide implementation priorities, align workflows, and evaluate Epic consulting partners effectively.
Core Clinical Care Modules
EpicCare Ambulatory
EpicCare Ambulatory is the foundation of Epic’s outpatient platform. It supports comprehensive visit documentation, e-prescribing, and results review for primary and specialty clinics. SmartTools such as SmartPhrases and SmartTexts streamline documentation, while specialty-specific templates improve note accuracy. Integration with MyChart enables direct patient communication and appointment management.
EpicCare Inpatient (ClinDoc)
ClinDoc powers inpatient documentation for nurses, physicians, and care teams. It captures assessments, progress notes, medication administration, and discharge planning. Decision support tools guide clinical care, and Rover mobile integration enables bedside charting. ClinDoc forms the core of hospital documentation and is one of the first modules implemented in Epic go-lives.
ASAP Emergency Department
ASAP is designed for emergency departments managing rapid patient throughput. It features a real-time track board, triage workflows, time-stamped documentation, and critical condition alerts. Integration with order sets and best practice advisories supports fast, evidence-based decision-making and seamless transitions from ED to inpatient care.
OpTime and Anesthesia
OpTime manages surgical scheduling, case documentation, and OR logistics, while Anesthesia captures intraoperative vitals, medication administration, and recovery data. These modules work together to streamline perioperative workflows, improve charge accuracy, and enhance patient safety across surgical services.
Stork Obstetrics
Stork supports pregnancy and delivery care, connecting prenatal documentation, labor tracking, and postpartum follow-up. Integration with fetal monitoring devices and newborn records ensures a continuous care experience for both mother and baby.
Ancillary and Specialty Modules
Beacon Oncology
Beacon supports chemotherapy and cancer care management. It standardizes protocols, monitors cumulative drug dosing, and integrates with Willow Pharmacy for accurate medication tracking. Oncology teams use Beacon to manage treatment plans and ensure patient safety throughout therapy cycles.
Cupid Cardiology
Cupid unites diagnostic and procedural cardiology data. It supports echocardiography, cardiac catheterization, and electrophysiology documentation, integrating directly with PACS for image management and structured reporting.
Radiant Radiology
Radiant serves as Epic’s radiology information system, handling scheduling, image tracking, and result distribution. It automates follow-up workflows and integrates with diagnostic imaging systems for seamless results review.
Beaker Laboratory
Beaker provides a complete laboratory information system for both clinical and anatomic pathology. It supports specimen tracking, quality control, and automated result delivery. Integration with other Epic modules ensures test results appear instantly in provider workflows.
Willow Pharmacy
Willow centralizes medication management across inpatient and outpatient settings. It integrates with dispensing cabinets, supports e-prescribing, and provides drug interaction alerts. This module is essential for safe, closed-loop medication administration.
Bugsy Infection Control
Bugsy automates infection prevention and regulatory reporting. It monitors lab data for early signs of infection, identifies isolation needs, and tracks healthcare-associated infection metrics for compliance and safety improvement.
Access and Revenue Cycle Modules
Prelude and Grand Central
Prelude manages patient registration and insurance verification, while Grand Central handles admissions, transfers, and discharges. Together, they provide the foundation for patient access, identity management, and accurate billing downstream.
Cadence Scheduling
Cadence optimizes provider scheduling and patient access. It supports provider templates, self-scheduling through MyChart, and automated rescheduling via Fast Pass. Efficient scheduling improves throughput and provider utilization.
Resolute Professional and Hospital Billing
Resolute manages both facility and professional billing. It automates charge capture, claim creation, and denial management. Integration with clinical modules ensures accurate reimbursement and financial transparency.
Charge Router
Charge Router links clinical documentation to billing. It validates and routes charges from source modules like OpTime, ClinDoc, and Radiant, reducing manual work and ensuring compliance.
Tapestry Managed Care
Tapestry supports organizations operating managed care or value-based contracts. It manages member eligibility, claims adjudication, and network relationships while linking financial and clinical performance metrics.
Patient Engagement and Mobile Tools
MyChart Patient Portal
MyChart provides patients with secure online access to their health information. Patients can view results, request refills, message providers, and pay bills through desktop or mobile apps. The portal supports digital engagement and continuity of care.
MyChart Bedside
MyChart Bedside extends engagement to inpatients through tablets displaying schedules, test results, and educational materials. It enhances patient experience and communication during hospitalization.
Haiku, Canto, and Rover
Haiku and Canto enable mobile access for physicians, while Rover supports nurses and ancillary staff with barcode medication administration and real-time documentation. These apps improve efficiency by bringing the EHR directly to the point of care.
Analytics and Population Health
Healthy Planet
Healthy Planet supports population health management and value-based care initiatives. It identifies at-risk patients, tracks quality measures, and integrates care management workflows. Organizations use it to manage chronic conditions and meet ACO goals.
Cogito and Caboodle
Cogito is Epic’s analytics engine, and Caboodle is its enterprise data warehouse. Together, they enable real-time dashboards, predictive analytics, and operational reporting. These modules help executives monitor performance and make data-driven decisions.
SlicerDicer
SlicerDicer allows clinicians and analysts to create self-service reports and explore data visually. It is commonly used for quality improvement, research, and operational trend analysis without the need for advanced technical skills.
Interoperability and Integration
Care Everywhere
Care Everywhere facilitates the secure exchange of health information between Epic and non-Epic organizations. It supports query-based and push-based record sharing, ensuring that patient data follows the individual across health systems.
Epic on FHIR
Epic’s FHIR APIs enable third-party app integration. These standards-based connections support innovation in patient engagement, remote monitoring, and analytics without compromising security.
EpicCare Link
EpicCare Link provides community partners with web-based access to patient data. It strengthens referral coordination and collaboration with external physicians, improving continuity of care.
Implementation Sequencing for Health Systems
Most health systems implement Epic in a phased approach that prioritizes operational stability and clinical adoption. A typical sequence includes:
-
Core Access and Registration: Prelude, Grand Central, Cadence
-
Foundational Clinical: EpicCare Ambulatory, EpicCare Inpatient, ASAP
-
Perioperative and Pharmacy: OpTime, Anesthesia, Willow
-
Ancillary Systems: Beaker, Radiant, Cupid, Beacon
-
Revenue Cycle: Resolute, Charge Router, Tapestry
-
Patient Engagement: MyChart, MyChart Bedside
-
Analytics and Population Health: Healthy Planet, Cogito, SlicerDicer
-
Mobile and Integration: Haiku, Canto, Rover, Care Everywhere, FHIR APIs
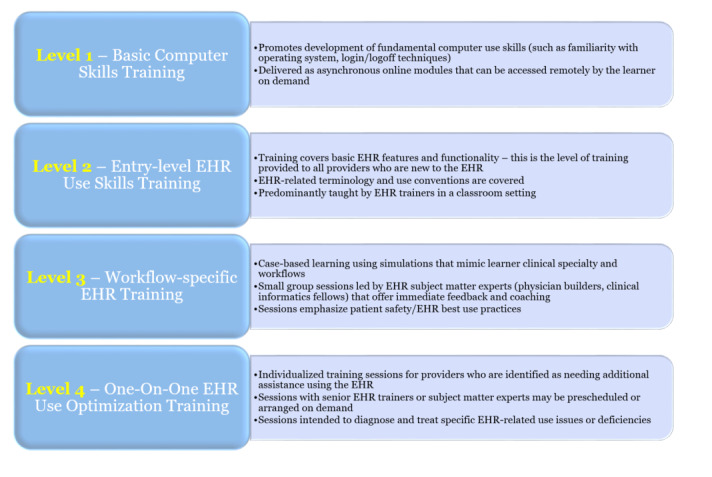
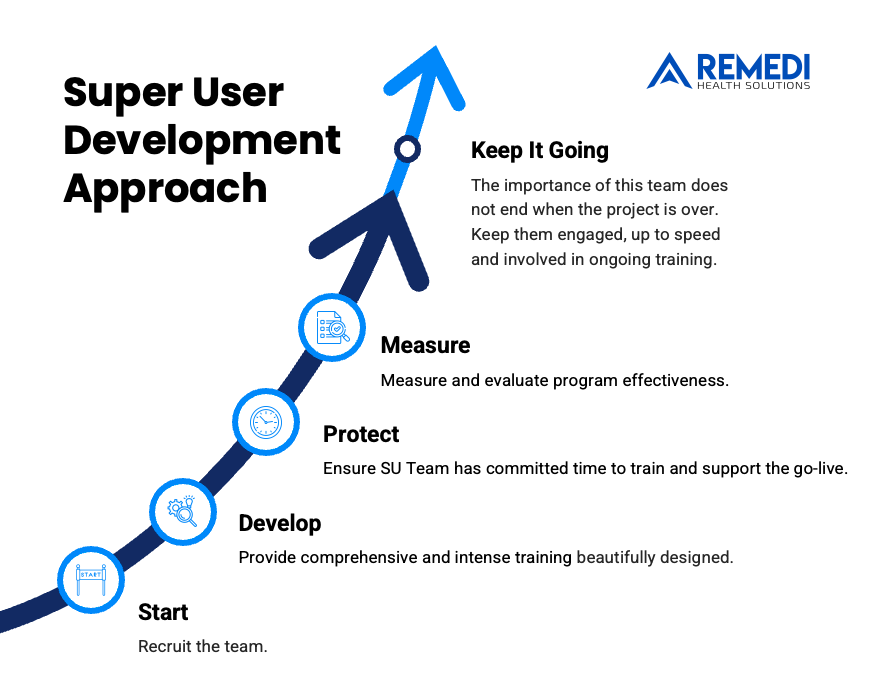
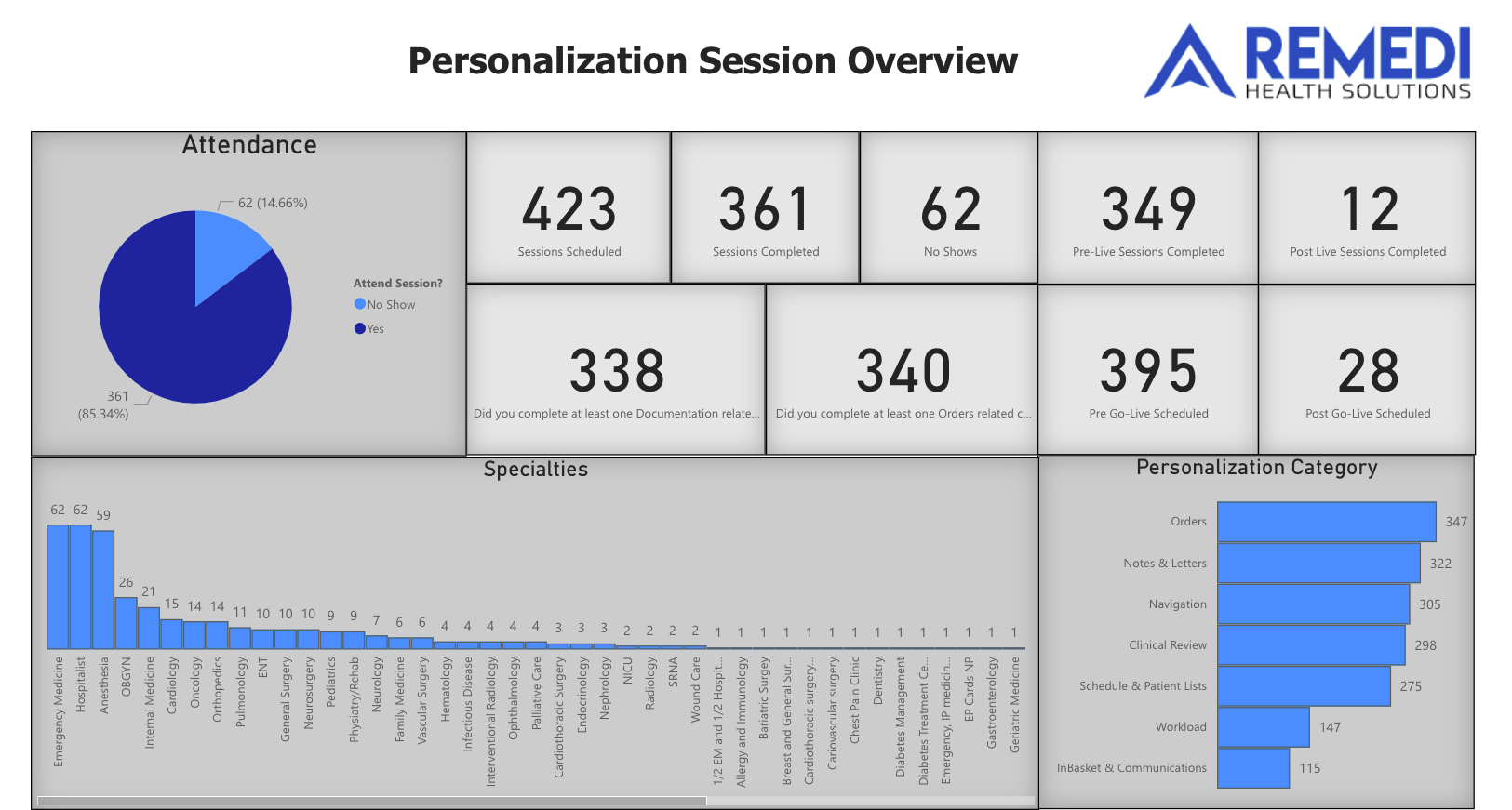
Strong Epic consulting guidance ensures each phase aligns with organizational readiness, governance structures, and clinical workflow design. Experienced consultants help tailor training programs, build personalization strategies, and measure adoption through Epic’s Signal data and reporting dashboards.
The Role of Epic Consulting
Effective Epic implementation depends on more than technology. Success comes from aligning system capabilities with clinical workflows and organizational goals. Epic consulting partners bring deep knowledge of system configuration, change management, and physician engagement. They help ensure that teams are trained, workflows are optimized, and adoption metrics are measurable and sustainable.
Conclusion
Epic’s ecosystem spans every dimension of healthcare operations, connecting patient access, documentation, analytics, and engagement within one platform. Understanding how each module fits together enables leaders to prioritize investments, streamline workflows, and improve outcomes.
Health systems that approach implementation strategically—and partner with experienced Epic consulting teams—achieve stronger adoption, better clinician satisfaction, and sustainable improvements in care quality and efficiency. Engaging consultants who understand both the clinical and operational sides of Epic ensures that technology truly enhances care delivery.