
Articles, Epic, Healthcare, Leadership April 10, 2024
After Leading Epic Go-Lives for over 15 Years, here’s what we’ve learned.
Updated August 2025 by ReMedi Health Solutions
At ReMedi Health Solutions, our decades of experience leading Epic implementations have taught us invaluable lessons about ensuring successful go-lives. From taking a clinical-first approach to engaging end-users and investing in comprehensive training, we’ve honed in on best practices that drive Epic adoption, efficiency, and better care delivery. Below are some non-exhaustive insights we’ve collected over the years from a healthcare executive’s perspective.
Epic Go-Live Lessons Learned from a Physician Executive
Lesson One. Solve clinical first, then IT.
For health IT leaders, one of the biggest decisions is determining how to optimize clinical workflows within Epic to support superior care delivery and revenue cycle management. All too often, the technical capabilities drive decisions rather than clinical needs.
For a health system that is transitioning from, merging, or acquiring a practice using an EHR like Cerner, Allscripts, or Meditech and going live on Epic, it’s critical to understand the ins and outs of both systems at the outset of the migration project. Using a strategic Change Management approach, it’s vital to know deeply how clinical workflows facilitated care on Cerner and how they will be optimized using Epic. Implementing new workflows across the entire system is difficult, but possible when the leadership team can explain both systems.
At ReMedi, we advocate a clinical-first philosophy. This means understanding and seamlessly integrating Epic into existing workflows for each role – from physicians to nurses, to billing specialists. Training staff to the top of their licensure by role allows them to practice at their highest level within Epic’s functionality.
We approach Epic solely through a clinical lens first, before examining the technical/IT requirements. Solutions are built around enhancing medical practices and decision-making capabilities, not structured around Epic system specs. For any issues that arise, our physician informaticists determine whether they stem from functionality gaps requiring optimization or necessitate system builds/integrations.
Lesson Two. Engage your end-users early and often.
One key challenge health IT leaders face is achieving buy-in and adoption from frontline clinical staff. Epic go-lives are major transformations – without end-user engagement, satisfaction plummets. According to a recent 2024 Arch Collaborative report, some examples of the tops methods that improve EHR satisfaction include:
- Making EHR education more accessible to all clinicians and staff
- Prioritizing effective communication with clinicians
- Involving clinicians in the EHR decision-making process
- Working closely with vendors to address challenges
- Promoting clinician well-being
From the start, ReMedi emphasizes consistent communication and incorporating feedback from doctors, nurses, care teams and administrators. We make them partners, not recipients, fostering a sense of control over the Epic implementation. This cultivates organizational investment and overall culture change.
The effects of end-user engagement on Epic adoption are tangible – when staff feel their voices are truly heard, there is a stronger sense of team cohesion and ownership over the success of implementing Epic. This personal stake translates to higher satisfaction ratings and adoption rates.
Lesson Three. Training is everything: build an army of super-users.
No amount of Epic functionality matters if staff aren’t trained comprehensively on leveraging those tools. Yet creating a structured, effective training program is one of the most complex decisions health IT leaders face.
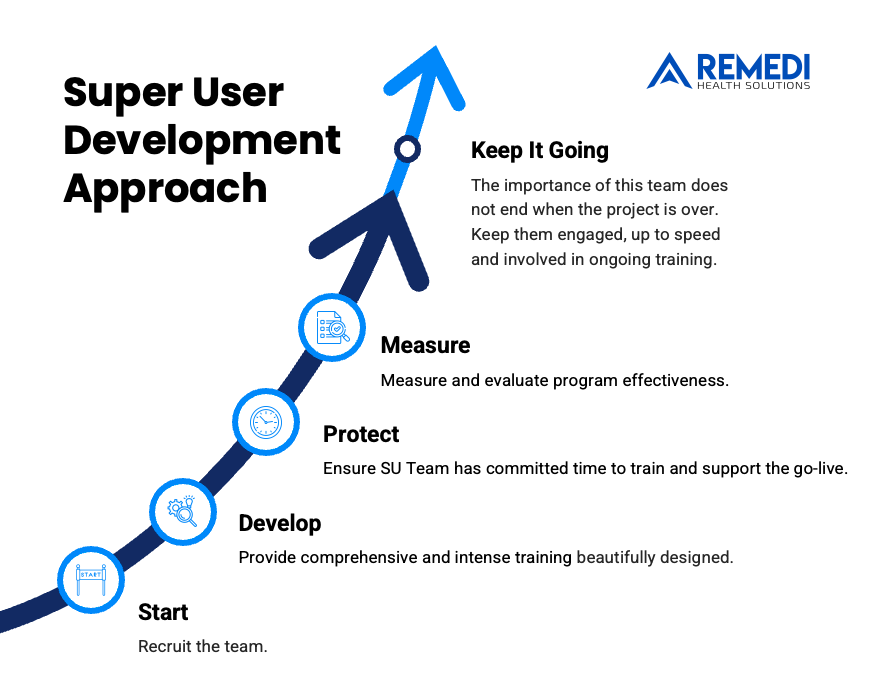
At ReMedi, we advocate developing a multi-pronged training program for a frictionless go-live. This includes immersive classroom sessions, web-based training resources, and most importantly, building an army of super-users. This approach has proven to foster trust, boost adoption rates, and maximize the long-term return on your Epic investment.
Empowering a dedicated group of end-users with in-depth training and ongoing support creates a core group of internal champions. These super-users, familiar with your organization’s culture and workflows, become in-house experts and resources for their peers throughout implementation and beyond.
By providing super-users with advanced Epic training and developing their skills as educators, healthcare organizations create reliable support systems. Staff have a trusted network of peers to turn to for issue resolution and continued optimization of Epic use.
Lesson Four. Epic Personalization is critical, especially for physicians.
Physician burnout and Epic dissatisfaction are well-documented challenges in the era of electronic records. Epic interruptions and administrative burdens are often cited as root causes.
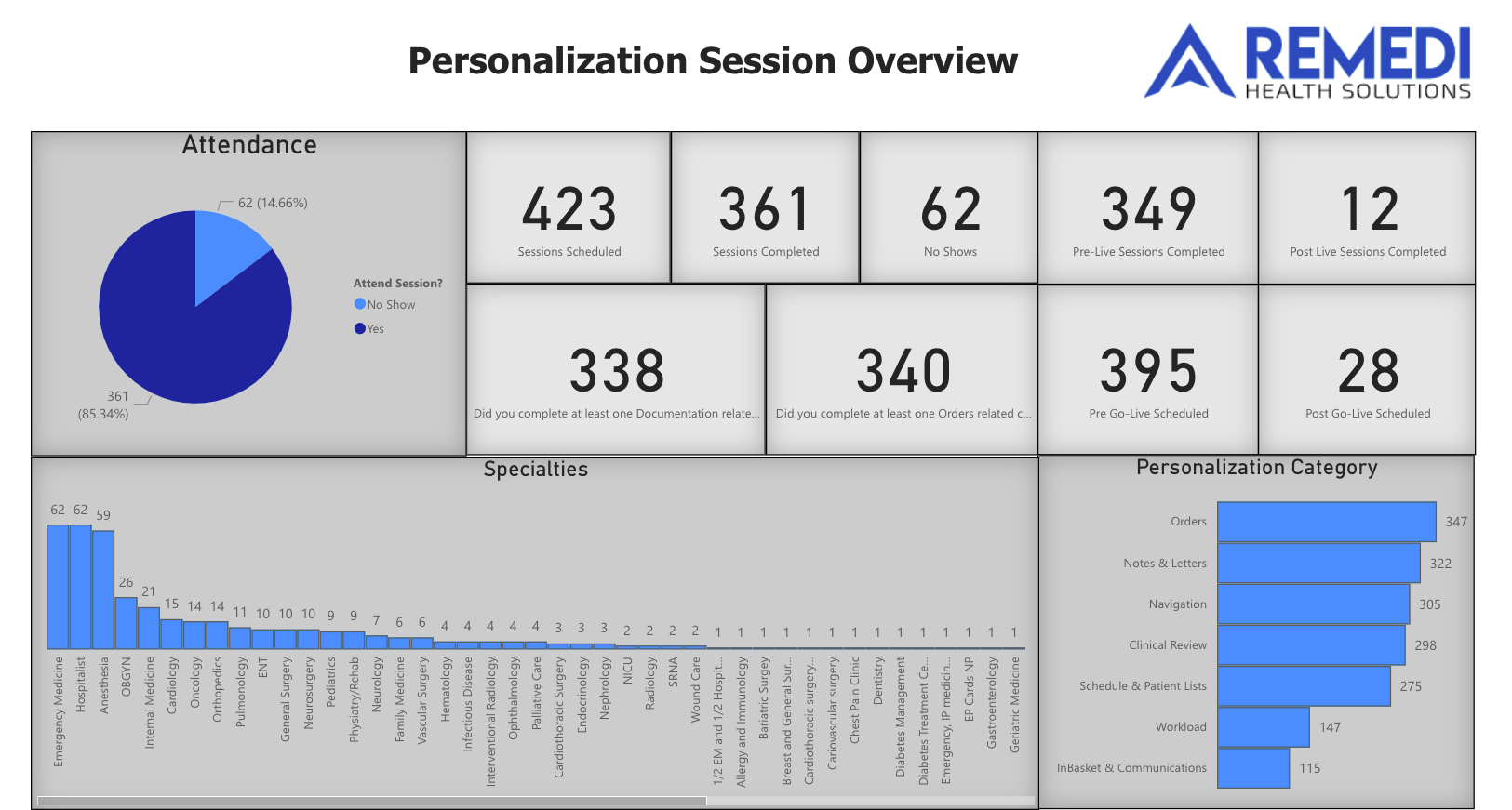
However, ReMedi’s approach illustrates how proper personalization and optimization can instead make Epic a productivity multiplier for doctors. We provide functional Epic training tailored specifically for physicians, so they understand the tools geared towards their specialty and responsibilities.
Inside of personalization and physician efficiency sessions, we unlock powerful Epic capabilities like smart phrases, order sets, and preference lists – all personalized to each doctor’s unique speciality and workflows. These shortcuts and efficiency hacks save physicians significant time per patient encounter. Rather than being a burden, Epic becomes streamlined for their workflow.
Furthermore, by pairing doctors with ReMedi’s physician informaticists specialized in their clinical area, we shed light on new ways to maximize the potential of Epic across the continuum of care. Doctors gain an enlightened perspective on Epic’s full potential directly from peers who have optimized the system for their respective field.
Lesson Five. The investment paradox: spend now or pay later.
Perhaps the biggest decision for health IT leaders is determining the optimal level of investment for Epic go-live and optimization efforts. At-the-elbow support is an additional cost, requiring short-term staffing for hyper-personalized assistance as issues arise during an Epic Go-Live.
However, skimping on knowledgeable resources risks crippling issues, workforce frustration, and sub-optimal Epic facilitated care down the line. ReMedi has found that implementing a hybrid model with both on-site and virtual support can optimize implementation costs without sacrificing quality. For an example of the outcomes from a hybrid Epic Go-Live, read this case study.
The investment paradox really comes down to taking a short-term perspective versus long-term view. While the upfront expenditure for comprehensive training, embedded resources, and persistent optimization is high, ReMedi has seen how this approach catalyzes positive impacts for decades in a healthcare system’s operations, clinician satisfaction, and quality of care metrics.
A major achievement upon going live on Epic is maintaining normal patient volumes and wait times from day one. We have found that patient data strategy plays a major impact on the ability to serve normal patient volumes during the Go-Live phase. We advise our health system partners that the optimal approach to optimizing patient data in Epic not only includes electronic conversion, but also data abstraction and chart preparation.
Patient data must be reconciled in Epic prior to a patient’s first visit in order to avoid “every patient feeling like a new patient” for clinicians. Working with a clinically trained, outsourced data team is an efficient method for health systems to achieve better data quality upon Go-Live at a sustainable cost.
Health IT leaders who take the plunge achieve instrumental wins – staffing costs decline as productivity skyrockets, medical errors reduce as decision support tools are maximized, and revenue cycles become more efficient and lucrative long-term.
By taking a clinical-centric approach, engaging staff as partners, providing multi-layered training, personalizing for providers, and making a focused investment, healthcare organizations can revolutionize the delivery of quality care using Epic. ReMedi’s 15+ years implementing this blueprint have proven these strategies overcome even the most daunting implementation challenges.
To meet with ReMedi’s talented Physician Executives about Epic, contact us here.
Frequently Asked Questions (FAQs)
What is the most crucial philosophy for a successful Epic EHR implementation?
The most crucial philosophy is a “clinical-first” approach. This means prioritizing the optimization of clinical workflows and enhancing medical practices and decision-making capabilities, rather than letting technical capabilities drive decisions. Solutions should be built around the needs of physicians, nurses, and billing specialists, ensuring Epic seamlessly integrates into their existing workflows and allows them to practice at the top of their licensure.
Why is end-user engagement vital for Epic go-lives?
End-user engagement is vital because Epic go-lives are major transformations, and without buy-in from frontline clinical staff, satisfaction and adoption rates plummet. By consistently communicating with and incorporating feedback from doctors, nurses, and care teams, they become partners in the implementation process. This fosters a sense of control, organizational investment, and a stronger team cohesion, leading to higher satisfaction and adoption rates.
How does comprehensive training contribute to a frictionless Epic go-live?
Comprehensive training is essential because no amount of Epic functionality matters if staff aren’t thoroughly trained to leverage those tools. A multi-pronged training program, including immersive classroom sessions, web-based resources, and especially the development of “super-users,” fosters trust and boosts adoption. Super-users, as in-house experts and educators, provide ongoing support and issue resolution, creating a reliable support system for their peers.
What is the significance of Epic personalization, particularly for physicians?
Epic personalization is critical, especially for physicians, to combat burnout and dissatisfaction often associated with electronic records. Tailored functional training for physicians, specialized to their unique workflows and specialties, unlocks powerful capabilities like smart phrases, order sets, and preference lists. This transforms Epic from a burden into a productivity multiplier, saving significant time per patient encounter and allowing physicians to maximize the system’s potential.
What is the "investment paradox" in the context of Epic go-lives, and how should it be addressed?
The “investment paradox” refers to the decision of optimal investment for Epic go-live and optimization. While upfront expenditure for comprehensive training, embedded resources, and persistent optimization is high, skimping on these resources risks crippling issues, workforce frustration, and suboptimal care down the line. A long-term view dictates that this initial investment catalyzes positive impacts for decades, including declining staffing costs, skyrocketing productivity, reduced medical errors, and more efficient revenue cycles. A hybrid model of on-site and virtual support can optimize costs without sacrificing quality.
How does a sound patient data strategy impact an Epic Go-Live?
A sound patient data strategy plays a major role in maintaining normal patient volumes and wait times from day one of a Go-Live. It’s crucial for patient data to be reconciled in Epic prior to a patient’s first visit. This includes not only electronic conversion but also data abstraction and chart preparation. Failure to do so can make “every patient feel like a new patient” for clinicians, hindering efficiency. Working with a clinically trained, outsourced data team can efficiently achieve better data quality.
What are some examples of services offered to optimize Epic EHR utilization post-implementation?
Post-implementation optimization services aim to enhance clinician satisfaction and maximize the EHR investment. These include Physician Efficiency Sessions (peer-to-peer EHR training and coaching), Specialty Specific Optimization (advanced training for unique challenges in specialty practices), and Quality Data Abstraction (post-Live efforts to improve data quality). These services ensure continuous improvement and adaptation of Epic to evolving needs.
What types of support are available during the initial Go-Live phase of an Epic implementation?
During the initial Go-Live phase, “at-the-elbow” support is crucial. This involves skilled, reliable specialists providing hyper-personalized assistance as issues arise from day one. Additionally, remote and virtual support through “Virtual EHR Services” can increase EHR adoption and address issues remotely. This immediate and accessible support helps clinicians navigate the new system, resolve problems quickly, and maintain productivity.
